
A root canal is a dental procedure that removes damaged or infected tissue from inside a tooth and seals the internal canals to prevent reinfection. This treatment preserves the outer tooth structure so you can maintain natural chewing function and avoid more extensive replacements. People typically need a root canal when deep decay, a crack, or trauma allows bacteria to reach the dental pulp and cause inflammation or infection.
Without treatment, an infected pulp can lead to increasing pain, swelling, and the spread of infection to surrounding bone or soft tissues. Root canal therapy aims to eliminate the source of infection, relieve pain, and restore the tooth so it can function normally for many years with proper restoration and care.
Your dentist will perform a clinical evaluation that includes a review of symptoms, a visual exam, and tests of tooth vitality to assess nerve status. Diagnostic X-rays are commonly used to view the extent of decay, the presence of an abscess, and the anatomy of the root system. These findings help distinguish reversible pulpitis, which may heal with conservative care, from irreversible pulpitis or necrosis that requires endodontic treatment.
Additional factors such as persistent spontaneous pain, prolonged sensitivity to temperature, swelling, darkening of the tooth, or pain on biting increase the likelihood that root canal therapy is indicated. The dentist will discuss the diagnosis and treatment options and explain the expected outcomes before proceeding.
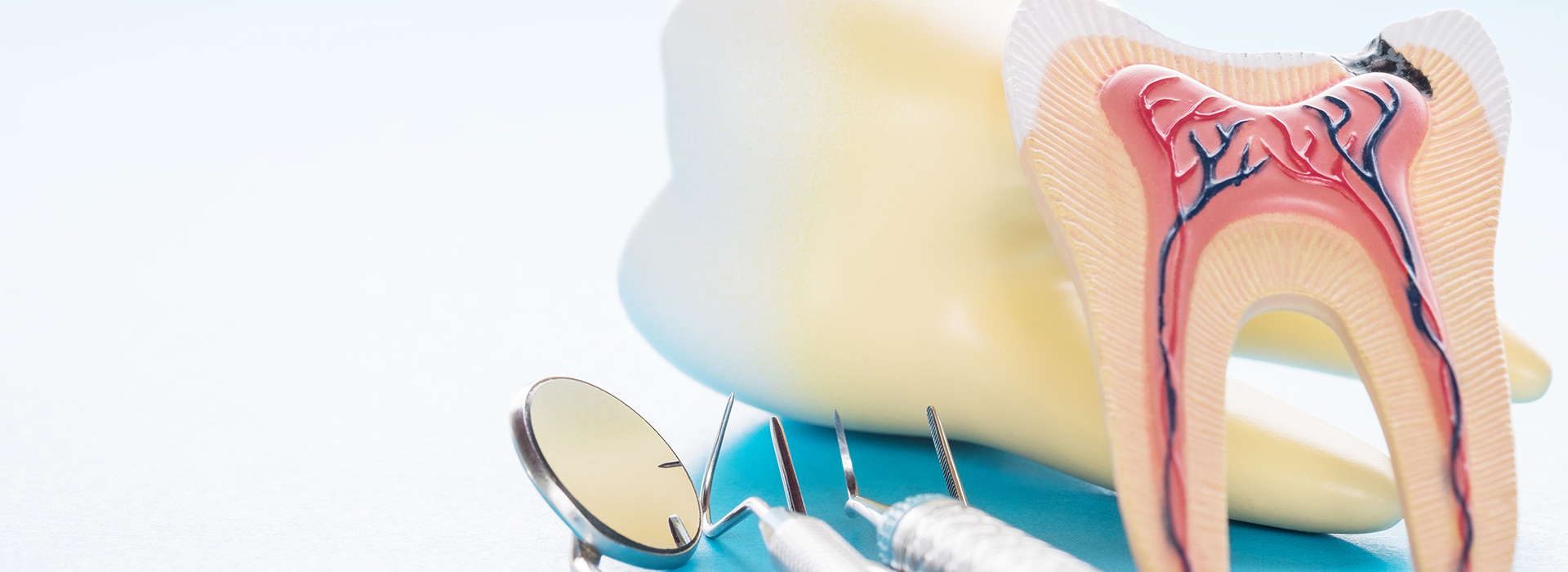
Modern root canal therapy is performed under local anesthesia so the treated tooth is numb and the procedure is comfortable for most patients. The dentist creates a small access opening, removes the inflamed or infected pulp, cleans and shapes the internal canals with precise instruments, and then fills and seals the canal space to prevent reinfection. Depending on the tooth and the level of infection, this can often be completed in a single visit or may require two appointments to ensure thorough cleaning.
After the canals are sealed, a temporary filling is placed if further restorative work is needed, and you will be advised on the timing for a permanent restoration such as a crown. The overall objective is to eliminate pain and infection while preserving as much natural tooth structure as possible to restore long-term function.
Thanks to advances in anesthesia and technique, most patients experience little to no pain during a root canal procedure and often report that it feels similar to receiving a filling. Mild soreness or tenderness in the surrounding tissues is common for a few days after treatment as the body heals. Over-the-counter pain relievers and any specific post-operative instructions provided by your dentist typically manage this discomfort effectively.
If significant pain, swelling, or other unexpected symptoms develop after treatment, contact the dental office promptly for evaluation. These symptoms can usually be addressed with a follow-up appointment, and early attention helps prevent complications.
Preparation for a root canal is straightforward: follow any pre-appointment instructions from your dentist, maintain regular oral hygiene, and bring a list of current medications and health conditions. If you have dental anxiety or medical concerns, discuss sedation options and medical history with the dental team ahead of time so they can recommend appropriate comfort measures. Eating a light meal before your appointment is advisable unless you and your provider have agreed on sedation that requires fasting.
Plan to allow time for follow-up care and for placement of a permanent restoration after the procedure if required. Arranging transportation is helpful if you use sedation that can affect coordination, and having someone available to assist you immediately after treatment can make recovery more comfortable.
After a root canal most patients return to normal activities quickly, with only mild soreness at the treated site for a few days. Your dentist will provide instructions on oral hygiene, temporary-restoration care, and medications if needed; following these recommendations helps prevent complications and promotes healing. Avoid chewing on the treated tooth until a permanent restoration is placed to reduce the risk of fracture.
Maintain routine dental checkups and cleanings so the dentist can monitor healing and the integrity of the final restoration. If you notice increasing pain, swelling, or signs of infection after treatment, contact the practice promptly for assessment and management.
Teeth that undergo root canal therapy are often more brittle and may require a protective restoration to restore strength and function. A crown is commonly recommended for posterior teeth or those with extensive structural loss because it helps distribute biting forces and reduce the risk of fracture. The dentist will evaluate the amount of remaining tooth structure and recommend the most appropriate restoration to protect the treated tooth long term.
In some cases a filling or an onlay may suffice, especially for smaller teeth with minimal damage. The timing of the final restoration is important; placing a definitive crown or restoration soon after endodontic treatment minimizes the risk of complications and improves the longevity of the tooth.
Root canal treatment is generally very successful, but like all medical procedures it carries some risks, including incomplete removal of bacteria, persistent infection, or canal anatomy that is difficult to treat. Some teeth have complex or curved root systems that require additional care or referral to a specialist for advanced endodontic techniques. Temporary post-operative symptoms such as mild pain or swelling are common and usually resolve with conservative care.
Rare complications include persistent infection that may require retreatment, surgical intervention, or, in some cases, extraction if the tooth cannot be preserved. Your dentist will explain potential risks based on your specific diagnosis and will recommend follow-up measures to monitor healing and address problems early if they arise.
Although the majority of root canal treatments succeed, failure can occur due to lingering bacteria, new decay, poor sealing, or complex root anatomy that was not fully cleaned. If symptoms recur or an X-ray shows persistent infection, options include nonsurgical retreatment to re-clean and re-seal the canals, an endodontic surgical procedure to address the root tip directly, or, if those measures are not feasible, extraction of the tooth. The appropriate choice depends on the tooth's condition, its restorability, and your overall oral health goals.
Your dentist or an endodontist will review imaging and clinical findings to recommend the most suitable approach. Timely intervention improves the likelihood of saving the tooth or selecting an alternative that preserves oral function and health.
Our team focuses on combining modern endodontic techniques with a patient-centered approach to make root canal therapy effective and as comfortable as possible. We use contemporary instrumentation, local anesthetics, and sterilization protocols to remove infection, seal canals, and prepare the tooth for a durable restoration. Communication about diagnosis, treatment steps, and post-procedure care helps patients feel informed and confident in their care experience.
After treatment, we help coordinate the placement of a final restoration and schedule follow-up visits to monitor healing and function at our Raleigh office. If a tooth presents complex anatomy or persistent issues, we discuss referral to a specialist so you receive the most appropriate care for a long-term, predictable outcome.

Ready to book your next appointment or have a question for our team? We're here to help.
Connecting with our team is simple! Our friendly staff is here to help with appointment scheduling, answer any questions about your treatment options, and address any concerns you may have. Whether you prefer to give us a call, send an email, or fill out our convenient online contact form, we’re ready to assist you. Take the first step toward a healthier, brighter smile – reach out to us today and experience the difference compassionate, personalized dental care can make.